Strabismus: Symptoms, Causes and Treatments
What is Strabismus?
Strabismus, also known as “crossed eyes” or “lazy eyes”, is the misalignment of the eyes, leaving a person with eyes that do not look straight. Worldwide, strabismus affects 1 in 50 individuals https://jamanetwork.com/journals/jama/fullarticle/2801812#google_vignette or approximately 4 percent of adults https://www.sciencedirect.com/science/article/abs/pii/S0039625713000866 and 3 percent of children. https://www.msdmanuals.com/professional/pediatrics/eye-defects-and-conditions-in-children/strabismus
Strabismus involves extraocular muscles, cranial nerves, supranuclear pathways and their cerebral controls. https://www.ncbi.nlm.nih.gov/books/NBK560782/ The condition can take on a vertical, horizontal, or torsional (multi-directional) misalignment.
People with strabismus lack binocular single vision, the ability to see a three-dimensional object with both eyes. Losing binocular single vision is very detrimental, according to ophthalmologist Dr. Srijana Adhikari, clinical advisory board member of Cure Blindness Project. “Losing binocular single vision means a person will lack depth perception and will be unable to judge distances when walking, playing sports or driving, and will be unable to optimally use tools such as a microscope. Images seen by the deviated eye get suppressed and the brain cannot process them.”
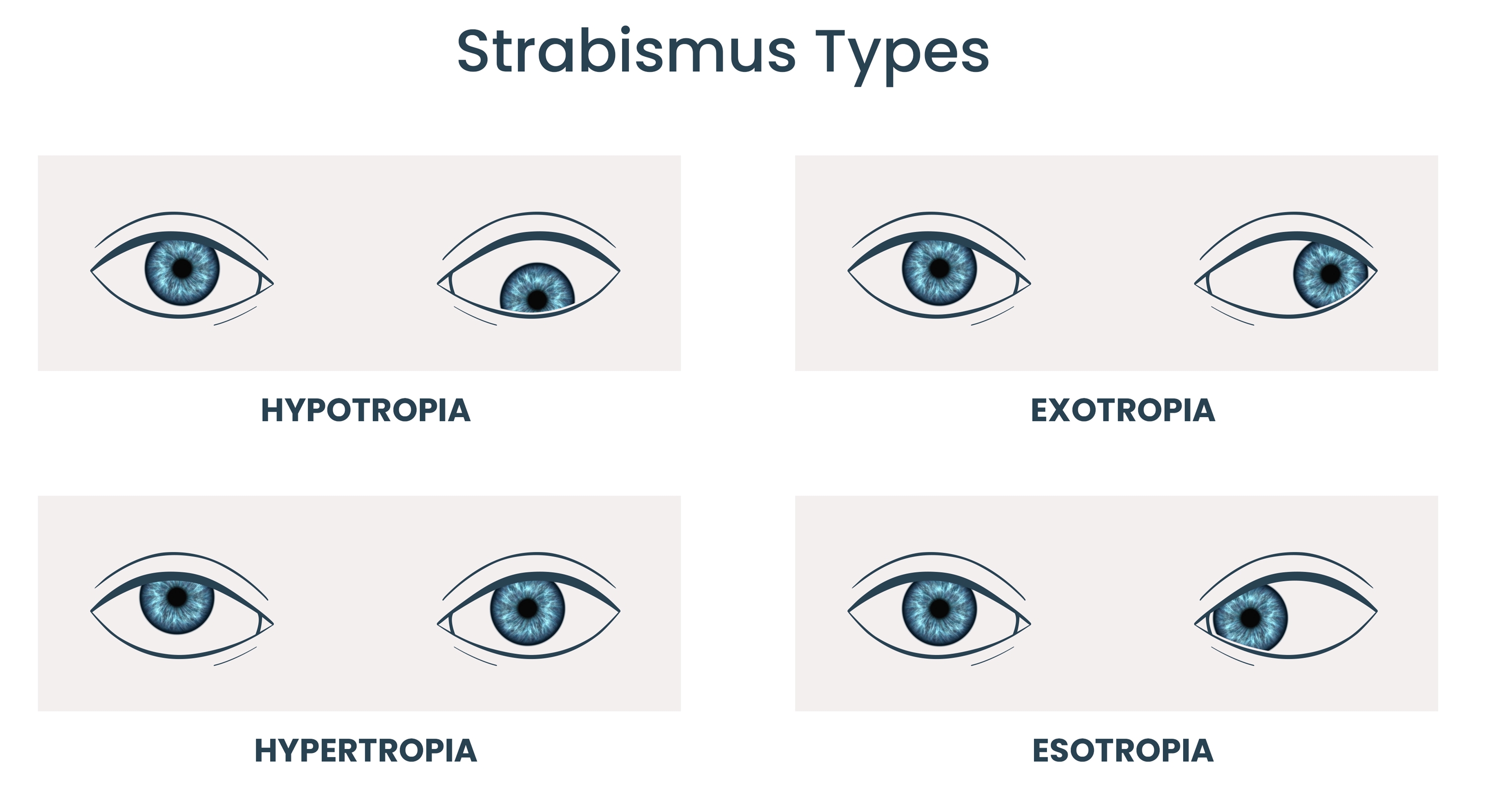
Types of Strabismus: Hypotropia, Hypertropia, Exotropia, Esotropia
“When we fail to develop the neurocircuitry of binocular single vision early in life, the results are strabismus and visual processing disorders,” notes Dr. Jason Cheung, a volunteer ophthalmologist with Cure Blindness Project.
What Causes Strabismus
When an eye starts to deviate, it may indicate another problem preventing good vision. “Whenever we do vision screening in children, we look for strabismus because it is a sign of something else going on inside the eye,” states Adhikari.

Those underlying conditions could be retinoblastoma https://pubmed.ncbi.nlm.nih.gov/34592118/ or a cataract. https://eyesurgeryguide.org/can-cataracts-cause-strabismus-understanding-the-link/ Thyroid disease https://www.aao.org/eye-health/diseases/what-is-strabismus might also be the culprit of crossed eyes, as might a traumatic injury https://www.aao.org/eye-health/diseases/what-is-strabismus or developmental delay. https://pubmed.ncbi.nlm.nih.gov/17313404/
Adhikari points out that strabismus can come from differences between the eyes; for instance, a severe refractive error or corneal scarring is present in just one eye, leading to strabismus.
Neurological complications can also be the source; cerebral palsy or a stroke https://www.aao.org/eye-health/diseases/what-is-strabismus can affect eye alignment. Adhikari notes that a specific nerve palsy of the eye is another cause, as it results in nerve paralysis which weakens one or more of the six extraocular muscles that keep the eye in position. This condition—paralytic strabismus—can happen in children, adults, and seniors.
Can Strabismus Be Corrected?
Strabismus treatment is primarily surgical, although both surgical and non-surgical approaches are used to make the eyes straight and to achieve binocular single vision, which means the eyes work together to provide meaningful depth perception.

Eye patching is one form of treatment for strabismus in children.

Eye patching is one form of treatment for strabismus in children.
The prognosis of strabismus is better when treatment happens sooner. The eyes are still developing until the age of seven or eight years old, so the possibility of saving single binocular vision is greater in younger patients. Treatment includes glasses, contact lenses, prism lenses, eye patching, medication, orthoptics exercises, or botox injections. https://www.webmd.com/eye-health/strabismus
“Patching and eye drops (atropine) before we do the strabismus surgery optimizes the neural function of the child’s lazy eye,” notes Cheung. These therapeutic approaches in the months leading up to surgery will lead to the best visual outcome for the child.
For strabismus left untreated until adulthood, strabismus surgery can align the eyes but binocular single vision will likely not be improved. “Later surgery has some functional benefits,” Cheung explains. “It may not be as effective as surgery done earlier in life, but it might allow the patients to retain some degree of their peripheral binocular vision which they may not have if the strabismus is never corrected.”
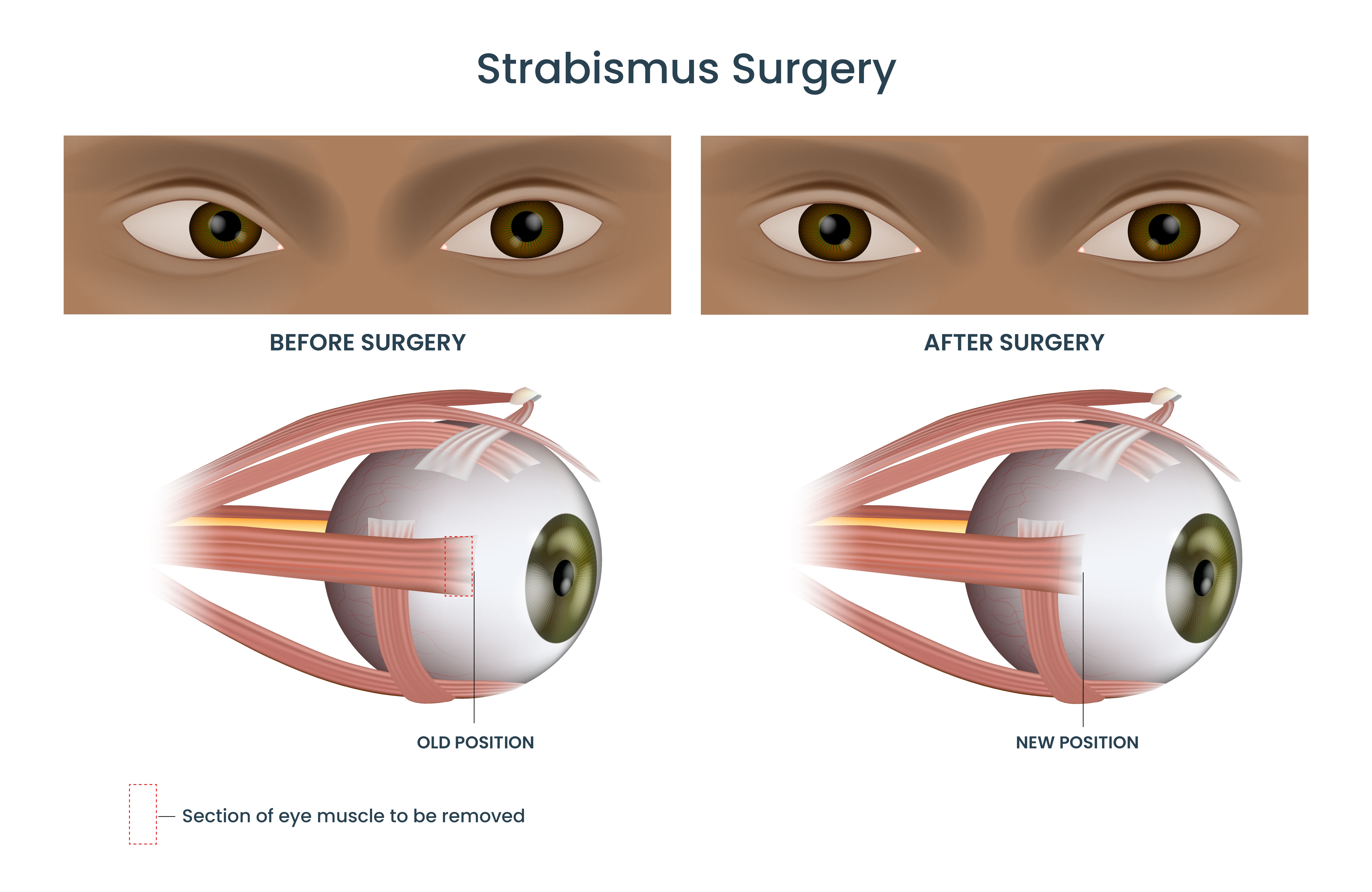
Diagram of the human eye showing section of muscle that may be removed in strabismus surgery.
All strabismus surgeries involve repositioning the extraocular muscles, loosening some muscles and tightening other muscles to make the eyes straight. The ophthalmic surgeon uses prisms to measure the deviation and then calculates precisely how much to move each muscle to correct the misalignment. Using surgical loupes and securing the extraocular muscles with non-absorbable sutures, the surgeon may disinsert, resect, and/or recess muscles for proper positioning.
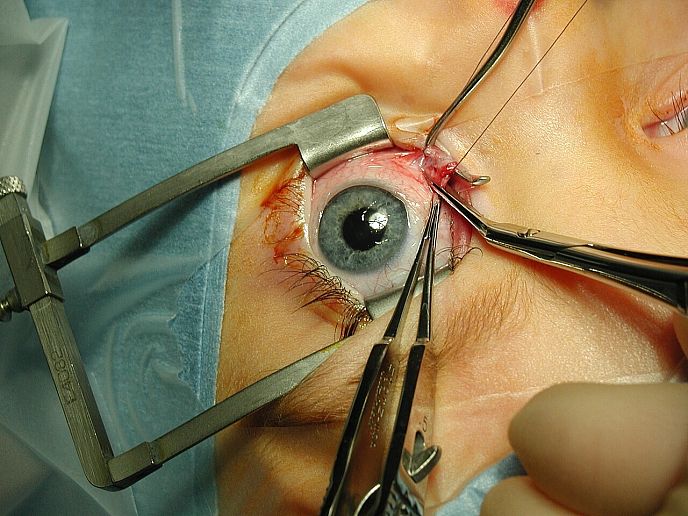
Strabismus surgery—medial rectus muscle being disinserted following pre-placement of vicryl sutures. Public Domain.
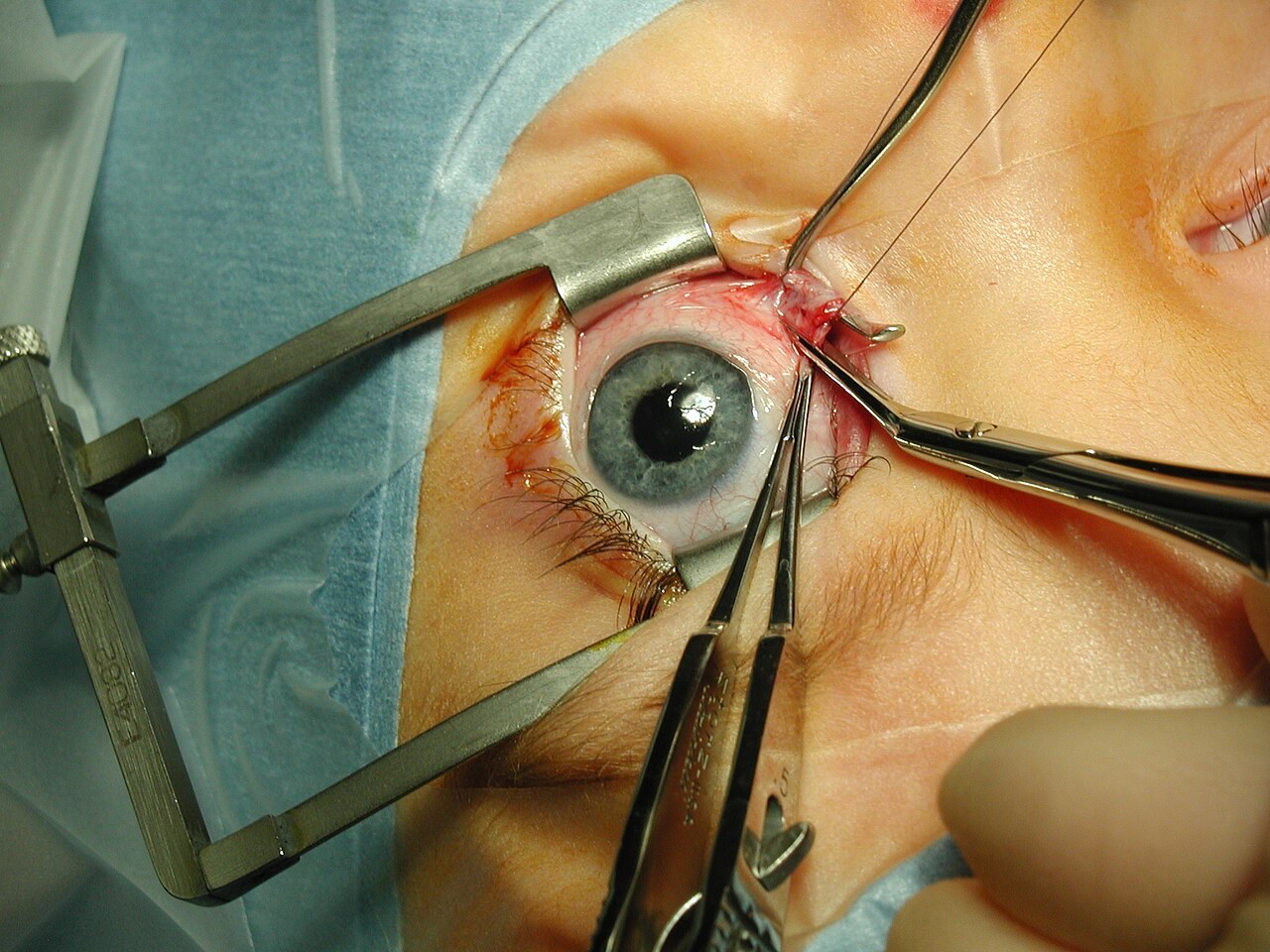
Strabismus surgery—medial rectus muscle being disinserted following pre-placement of vicryl sutures. Public Domain.
Anesthesia during strabismus eye surgery can be general or local. General anesthesia is used in strabismus surgery with children and is a customary practice for patients in the US and other countries. “For adult patients in low- and middle-income countries, medical teams anesthetize and immobilize the eye with a local anesthetic agent using a retrobulbar block, a customary practice in many countries,” explains Adhikari, “because of the cost and the high volume of the surgeries we do.”
“No matter the stage, strabismus can almost always benefit from surgery,” Cheung advises. Adhikari notes. “My youngest patient was a 6-month old child and my oldest was an 80-year-old man.”
Transient Strabismus
Transient strabismus, also known as intermittent strabismus, is a common presentation in infants and young children. https://www.webmd.com/eye-health/strabismus Crossed eyes can be constant, intermittent, or initially intermittent that later becomes constant.
“Parents usually notice that whenever the child is tired, daydreaming, or unfocused (having just woken from sleep), his or her eyes may drift,” Adhikari comments. “We watch the condition to see if it progresses to constant strabismus.”
One condition, pseudostrabismus, looks like strabismus but is not. The facial structure of children— their flat nasal bridge and prominent eyelid folds—give the illusion that one eye looks esotropic (eyes turn inward). “Many parents bring those children to us thinking that it's strabismus,” explains Adhikari, “and we can give them good news that it is not.”

5-year-old Heran Tsega received surgery for strabismus from a Cure Blindness Project volunteer pediatric ophthalmologist. Her mother expressed her gratitude and shared, “Thank you to the doctors and to Cure Blindness Project for giving my daughter this surgery.” Read her story.
Strabismus Stigmas
In many cultures, crossed eyes or a wandering eye is considered a defect. Strabismus may carry the social stigma that someone is less intelligent or a bad marriage prospect.
Even with no cultural stigma, strabismus affects personal communication. “You look at somebody with strabismus and you do not know which eye to look at when you are having social interactions,” states Cheung. Self-esteem issues and psychosocial consequences are associated with the condition.
“By doing the surgery—even later on in life—you confer some degree of functional benefit and psychosocial benefit,” says Cheung. “Studies show that, even in North America, patients with strabismus are perceived as less honest. They are hired less often because of their eye misalignment.”
By contrast, strabismus in Nepal was considered a sign of good luck in the past. “If your child had a strabismus, it meant the child would succeed in life or good things would happen to the family,” notes Adhikari. “That misconception has changed due to awareness of strabismus. Our vision screenings include teaching parents that one sign of poor vision is strabismus.”
Challenges of Treating Strabismus in Low and Middle Income Countries
To cure strabismus, overcoming these challenges in low- and middle-income countries is crucial:
- Local capacity needs: Continuing medical education, and well skilled and qualified anesthesiology support
- Infrastructure and equipment needs: Equipment for general anesthesia and precise eye measurements
- Comprehensive patient care: Access to subspecialty services, patient and family counseling, follow-up with treatment plans, and post-operative care
- Scale of prevention efforts: Increased community awareness and more vision screenings for early detection
In Ethiopia and Ghana, foundational ophthalmology services are available, but the extensive specialized services required for pediatric ophthalmology care are not as available as they are in higher-income nations. As Head of Pediatric Ophthalmology and Strabismus at Tilganga Institute of Ophthalmology in Nepal, Adhikari sees this firsthand. “Lack of awareness and education means we need to go to communities as much as possible with vision screening programs to detect strabismus in a timely manner. If the treatment is not started before five or six years of age, children can be visually impaired for their whole life.”
Lack of awareness and education means we need to go to communities as much as possible with vision screening programs to detect strabismus in a timely manner. Dr. Srijana Adhikari
How Cure Blindness Project is Treating Strabismus
Globally 148 million people have strabismus https://www.sciencedirect.com/science/article/abs/pii/S0039625721000783 and all of this burden is treatable. Cure Blindness Project, a global non-profit organization, working towards treating strabismus in underserved communities in 30 nations across sub-Saharan Africa, South Asia and South America.

Dr. Srijana Adhikari and Dr. Kumale Tolesa performing surgery for strabismus in Nepal.

Dr. Srijana Adhikari and Dr. Kumale Tolesa performing surgery for strabismus in Nepal.
Cure Blindness Project’s model begins with bringing high quality care to those who need it and continues to address strabismus (crossed eyes) through preventative measures and by establishing highly qualified, well-trained local capacity.
Cure Blindness Project volunteer ophthalmologists and partners have performed approximately 1.8 million sight restoring surgeries, including those for strabismus. For early detection and treatment of strabismus and other eye disease, Cure Blindness Project has conducted more than 19.1 million eye screenings. The organization emphasizes self-sustainability through strengthening ophthalmology residency programs for local and international pediatric ophthalmologists by training them in strabismus surgery through Tilganga Institute of Ophthalmology and other medical centers in Nepal, Ghana, Ethiopia, and Bhutan.






